Why Syndromic Surveillance Is More Accurate Than Other COVID-19 Tests
By: Dr. Sarma Velamuri, M.D., Natalie Cheng, D. Maneesh Kumar, D.O., Ph.D., FAAP
Imagine this: Bob wakes up one morning and starts to not feel well. He has a cough, fever, body aches, and anosmia. Bob should probably just take some over-the-counter medicine and then rest. Normally, he would be back to himself in a few days. However, with the ongoing pandemic, everyone is now on edge when they develop these symptoms. Bob has to worry about not infecting others and since he works at a meatpacking plant, he doesn’t want the whole plant to shut down if he ends up going to work and testing positive for coronavirus. So, he goes and gets tested. The result comes back saying he does not have COVID-19.
Bob goes to work. The PCR test result is wrong, and he infects 30 other people.
Unfortunately, PCR tests may miss more than 1 in 5 COVID-19 cases as you’ll see below in the Annals of Internal Medicine article.
AAFP’s guide for physicians states, “The molecular test is much more specific, but false negatives do occur. Use clinical judgement and continue to treat the patient as positive if symptomatic or if there was a known exposure.”
If you have enough data on symptoms (I.e. syndromic surveillance data), you don’t need the PCR test.
As shown by the colleagues at Johns Hopkins published in Annals of Internal Medicine, using PCR testing to “rule out” symptomatic patients is very risky.
A person reporting symptoms who gets tested on:
-
Day #1 with a negative PCR test: 18% to 65% chance the test is wrong
-
Day #3 with a negative PCR test: 20% chance the test is wrong
Bottom line: For a person who has a constellation of symptoms with a negative PCR test, believe the symptoms not the negative PCR test.
At this point, you may be wondering: is there a way to improve accuracy and better diagnose patients since widespread population testing is still not available in all countries?
Syndromic Surveillance
The short answer is yes. If you haven’t heard already, COVID-19 is an acute respiratory illness caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In order to correctly diagnose this illness, you would have to identify the combination of symptoms that are most predictive of COVID-19. Nature, a leading weekly, international scientific journal, recently published research on how real-time tracking of self-reported symptoms can predict potential COVID-19. What they are describing is a concept called syndromic surveillance. According to the Journal of the American Medical Informatics Association, “syndromic surveillance refers to methods relying on detection of individual and population health indicators that are discernible before confirmed diagnoses are made. In particular, prior to the laboratory confirmation of an infectious disease, ill persons may exhibit behavioral patterns, symptoms, signs, or laboratory findings that can be tracked through a variety of data sources.”
In the report from Nature, the researchers had a total of 2,618,862 participants who reported their potential symptoms of COVID-19 on a smartphone app. They found that among the 18,401 who had undergone a SARS-CoV-2 test, 65.03% had reported a loss of smell and taste, which was higher for those with a positive test result than with a negative test result (21.71%).
Here’s the odds (OR = odds ratio) that someone who has lost their sense of smell has to test positive for COVID compared to other symptoms.
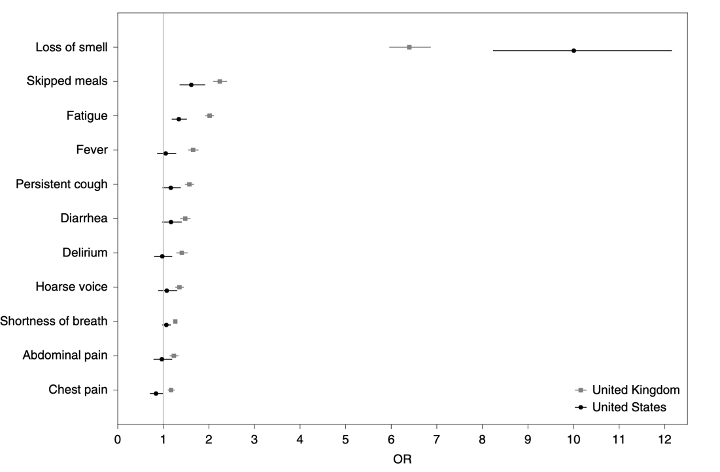
In addition to looking at anosmia, the researchers also ran tests to adjust for age, sex, and BMI to identify other symptoms that might be associated with SARS-CoV-2. They found all ten symptoms: fever, persistent cough, fatigue, shortness of breath, diarrhea, delirium, skipped meals, abdominal pain, chest pain, and hoarse voice to be associated with testing positive for COVID-19. From all the research conducted and regardless of any bias from mainstream media reports, the association between COVID-19 and loss of smell and taste remains strong.
Anecdotally, let’s revisit Bob’s story at the beginning.
Thankfully, Bob never infected everyone in his workplace. This type of event has happened in real life though.
Since his company has Quickscreen, Bob decides to answer a few questions in the tool before going into work. Bob opens the internet browser on his phone and goes through the questions. He fills out which symptoms he is currently experiencing and at the end of the process, he receives a red indicator noting that he has a high chance of having COVID-19. He contacts his HR department and they have already received his red results. The HR representative instructs Bob to stay home and monitor his symptoms so that he won’t infect others. Bob quarantines himself at home and continues to rest. A few weeks later, he starts to feel better and wants to see if he can go back to work. He answers the questions on the symptom tracker tool again before going into work and he receives a green certification. He doesn’t have any symptoms anymore and feels well enough to go back to work. He checks in with the HR representative and is cleared to go back to work.
Next Steps
What do you do now that you have started feeling unwell? For starters, if it’s a medical emergency, seek medical attention immediately. If you think you have been exposed to COVID-19 and develop a fever and symptoms, call your healthcare provider for medical advice. Continue to monitor your symptoms because they can be a major indicator of coronavirus. If you’re a business, school, or organization looking to track symptoms and want to better manage your employees, visitors, and vendors and prevent the spread of coronavirus, please reach out to us.
Remember to continue practicing good hygiene (ex. Washing your hands), maintaining social distancing, and wearing a mask correctly. Stay safe!