Why You Need To Consider Sepsis When Fighting COVID-19
By: Dr. Sarma Velamuri, M.D., Mihir Pethe
The CDC estimates sepsis kills 270,000 Americans each year, a figure that would put it as the third leading cause of death in the country and the #1 cause of death in US hospitals. Approximately 1 in 3 people who die in hospitals die of sepsis, though their cause of death is often misattributed to the original condition that hospitalized them. Sepsis is also the #1 cause of avoidable long-term medical complications.
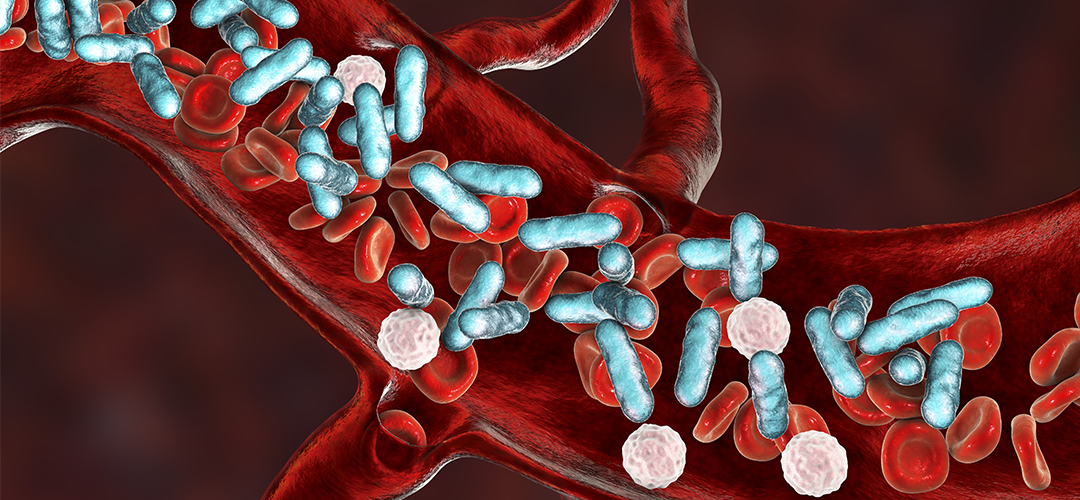
COVID-19 is the defining health story of this decade, yet despite the many headlines there is little recognition of how interlinked COVID-19 is with sepsis. The two are closely related, and in some ways COVID-19 could be viewed as sepsis caused by the SARS-CoV-2 virus. Sepsis is defined as “a potentially life-threatening condition caused by the body’s response to infection”. Many COVID-19 patients suffer organ damage outside of their respiratory system and severe COVID-19 manifests itself as multi-organ system failure, both of which suggest the patients are experiencing sepsis. In patients who died of COVID-19, 100% were found to meet the criteria for sepsis, and 70% met the criteria for septic shock.
The reasons for this close relationship between sepsis and COVID-19 are varied and still being understood. The SARS-CoV-2 virus is both more likely to cause sepsis than other viral diseases on its own, and more likely to cause secondary infections that may lead to sepsis.
It is clear, however, that clinicians and hospitals need to beware of sepsis when fighting COVID-19. Viral “sepsis” often proves far more difficult to fight than bacterial sepsis because of the relative lack of antiviral drugs that can be administered. Sepsis care without the right antivirals or antibiotics is focused on supporting the patient, rather than directly fighting the infection.
Secondary bacterial sepsis can occur due to prolonged ventilation or the use of immunosuppressant medications used to treat COVID-19. Hospitals need to detect this early and prevent it to achieve the best patient outcomes for their COVID patients. Additionally, if hospitals can predict which patients are going to end up on ventilators they can be safely intubated ahead of time without endangering nurses. Luminare can help identify patients who may be at the greatest risk and solve problems before they ever emerge.
Sepsis has long been underexamined and poorly prioritized by hospitals, clinicians, and researchers. COVID-19 has highlighted the need for all of us in the healthcare community to pay attention to this problem, work together to prevent sepsis, and combat it once it appears.
Have questions on sepsis and COVID? Feel free to reach out to us.
Sources Used: 1. The Relationship Between Sepsis and COVID-19: What We Know2. Can COVID-19 Cause Sepsis? Explaining the Relationship Between the Coronavirus Disease and Sepsis3. Coronavirus Disease 2019 Sepsis4. Sepsis and Coronavirus Disease 2019

![[Webinar] Sepsis Process Improvement in the COVID Era](https://no-cache.hubspot.com/cta/default/3043630/53a11dab-6a66-4c62-9cce-ee4b48468f86.png)
